Orthopedic Body Part Explorer
Select a body part category below to learn more about what orthopedic doctors treat:
Bones
Structural support & mineral storage
Joints
Facilitate movement
Muscles & Tendons
Generate & transmit force
Ligaments & Cartilage
Stabilize joints & cushion
Spine
Central support & flexibility
Ever wondered which parts of your body end up on an orthopedic doctor's treatment list? It’s not just your knee or hip - the scope covers everything that moves, bears weight, or supports your posture. Below we break down the exact anatomy an orthopedist handles, how they diagnose problems, and what treatment routes they typically use.
Understanding the Musculoskeletal System
Musculoskeletal system is a network of bones, joints, muscles, tendons, ligaments, and cartilage that enables movement and maintains structural integrity. When any component of this system falters, an orthopedist steps in. The system can be visualized as three interlocking layers: the hard framework (bones), the movable hinges (joints), and the soft movers (muscles, tendons, ligaments, and cartilage). Each layer has distinct health concerns, but they all influence one another.
Bones: The Rigid Foundation
Bones are living tissue that provides structural support, protects vital organs, and acts as mineral storage. Orthopedic doctors treat fractures, bone deformities, osteoporosis‑related collapses, and bone infections. Typical interventions range from casting or splinting for simple breaks to internal fixation using plates, screws, or rods for complex fractures. In cases of severe bone loss, procedures like bone grafting or the use of synthetic bone substitutes become necessary.
Joints: The Body’s Hinges
Joints are connections between bones that allow varying degrees of motion, from the ball‑and‑socket of the shoulder to the pivot of the neck. Orthopedists manage arthritis, dislocations, meniscal tears, and labral injuries. Treatment pathways include joint aspiration, corticosteroid injections, arthroscopic repairs, or joint replacement when cartilage loss is irreversible. A growing trend in 2024‑25 is the use of patient‑specific 3‑D‑printed implants that match the exact geometry of the joint.
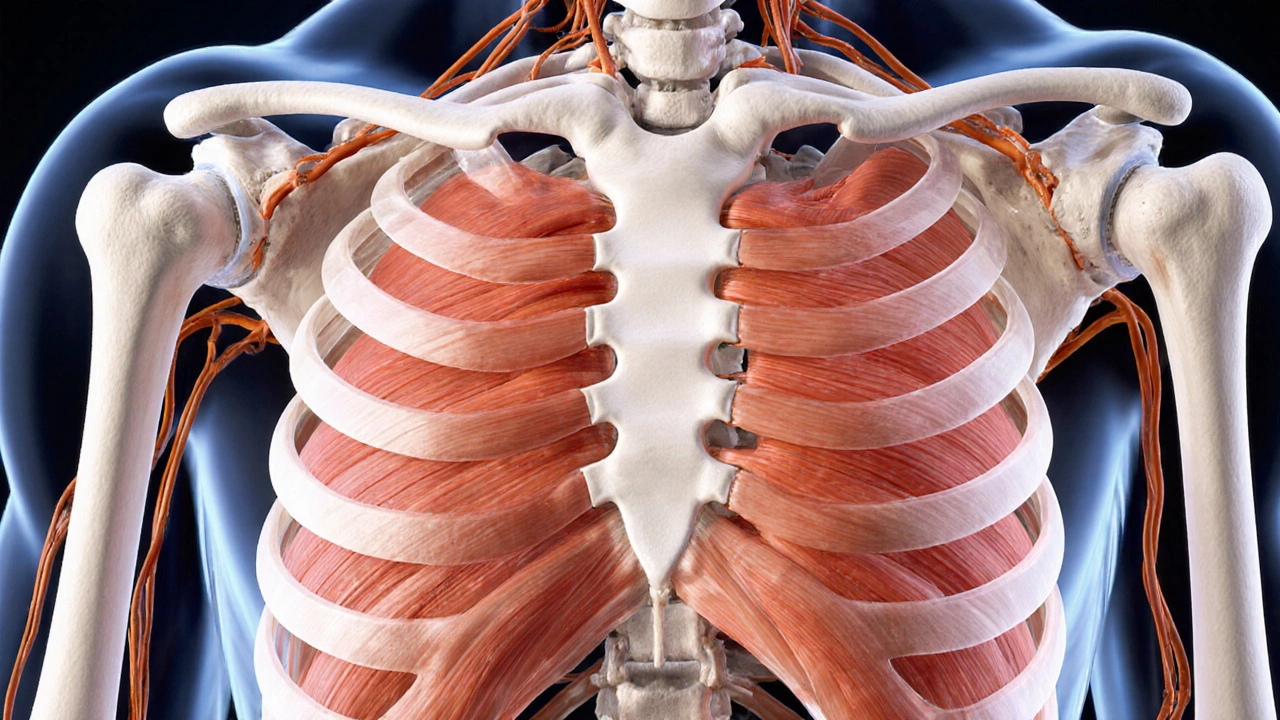
Muscles and Tendons: The Movers and Pullers
Muscles generate force, while tendons transmit that force to bones, enabling movement. Orthopedic doctors address strains, tears, and chronic tendinopathies such as Achilles or rotator‑cuff tendinitis. Non‑surgical options like eccentric strengthening programs, platelet‑rich plasma (PRP) injections, and shock‑wave therapy are common. If the tendon is ruptured, surgical repair with sutures or grafts restores continuity.

Ligaments and Cartilage: The Stabilizers
Ligaments bind bones together, preventing excess motion. Cartilage covers joint surfaces, reducing friction and absorbing shock. Injuries such as anterior cruciate ligament (ACL) tears or meniscal damage are frequent in athletes. Orthopedic surgeons often perform arthroscopic reconstruction for ligaments and partial meniscectomy or repair for cartilage defects. Emerging biologic options-stem‑cell injections and scaffold‑based cartilage regeneration-show promising early results.
The Spine: Central Support Column
Spine consists of vertebrae, intervertebral discs, ligaments, and surrounding musculature, providing both support and flexibility. Orthopedic care for the spine includes addressing herniated discs, spinal stenosis, scoliosis, and compression fractures. Treatments range from physical therapy and epidural steroid injections to minimally invasive decompression and instrumented fusion. In 2025, navigation‑assisted robotic spine surgery is becoming standard for precise screw placement.
Common Conditions Orthopedists Treat
- Arthritis: Osteoarthritis and rheumatoid arthritis cause cartilage breakdown; options include lifestyle modification, injections, and joint replacement.
- Fractures: From hairline cracks to compound breaks; treatment depends on fracture type, location, and patient age.
- Sports Injuries: ACL tears, rotator‑cuff tears, and stress fractures; managed with rehab, bracing, or surgery.
- Degenerative Disc Disease: Disc dehydration leads to pain; treated with physical therapy, disc replacement, or fusion.
Diagnostic Tools Used by Orthopedic Doctors
Accurate diagnosis starts with a thorough history and physical exam, followed by imaging. X‑rays reveal bone alignment, CT scans provide 3‑D detail for complex fractures, while MRI visualizes soft‑tissue structures like ligaments and cartilage. In 2024, the adoption of weight‑bearing MRI allows clinicians to see joint mechanics under load, improving treatment planning.

Treatment Spectrum: From Conservative to Surgical
Orthopedic care follows a stepwise approach:
- Conservative Management: Rest, physiotherapy, NSAIDs, orthotics, and activity modification.
- Interventional Therapies: Injections (corticosteroid, hyaluronic acid, PRP), nerve blocks, and arthroscopy.
- Surgical Intervention: Open or minimally invasive procedures, joint arthroplasty, spine fusion, and osteotomies.
The choice depends on injury severity, patient goals, age, and overall health. Today’s orthopedists also consider enhanced recovery pathways that reduce hospital stay to one day for many joint replacements.
When to See an Orthopedic Doctor
Consider scheduling an appointment if you experience any of the following:
- Persistent joint pain lasting longer than two weeks.
- Visible deformity, swelling, or bruising after an injury.
- Limited range of motion that interferes with daily activities.
- Neurological symptoms such as tingling or weakness linked to a specific limb.
Early evaluation can prevent chronic damage and speed up return to function.
Quick Takeaways
- Orthopedic doctors treat the entire musculoskeletal system - bones, joints, muscles, tendons, ligaments, cartilage, and spine.
- Common issues include fractures, arthritis, sports injuries, and spinal disorders.
- Diagnosis relies on physical exams plus X‑ray, CT, and MRI imaging.
- Treatment ranges from conservative rehab to advanced robotic surgery.
- Seek care early for pain, swelling, or loss of motion to avoid long‑term complications.
Comparison of Body‑Part Categories Treated by Orthopedists
| Part Type | Primary Function | Common Conditions | Typical Treatments |
|---|---|---|---|
| Bones | Structural support & mineral storage | Fractures, osteoporosis, bone infection | Casting, internal fixation, grafting |
| Joints | Facilitate movement | Arthritis, dislocation, meniscal tear | Injections, arthroscopy, joint replacement |
| Muscles & Tendons | Generate & transmit force | Strains, tears, tendinopathy | Physio, PRP, surgical repair |
| Ligaments & Cartilage | Stabilize joints & cushion | ACL tear, cartilage degeneration | Arthroscopic reconstruction, biologics |
| Spine | Central support & flexibility | Herniated disc, stenosis, fractures | Therapy, injections, fusion, robotic surgery |
Frequently Asked Questions
Which doctors treat back pain - orthopedists or neurosurgeons?
Both specialties manage spinal disorders, but orthopedists focus on bone‑related issues, mechanical instability, and joint degeneration, while neurosurgeons handle nerve‑root compression and complex spinal cord pathology. Often they work together to decide the best approach.
Can an orthopedic doctor treat hand and wrist problems?
Yes. Hand and wrist injuries - carpal tunnel, Scaphoid fractures, tendon lacerations - are routinely managed by orthopedists, sometimes in a dedicated hand‑surgery clinic.
Do I need a referral to see an orthopedist in Australia?
Public hospitals usually require a GP referral, but many private practices accept self‑referrals. Check your health insurance policy for coverage details.
What is the difference between an orthopedic surgeon and a sports medicine doctor?
Orthopedic surgeons perform operative procedures on bones and joints. Sports medicine physicians specialize in non‑operative care, injury prevention, and rehabilitation, though many also hold orthopedic surgical training.
How long does recovery typically take after a joint replacement?
Most patients achieve functional independence within 6‑12 weeks, with full activity levels returning by 4‑6 months under an enhanced recovery protocol.




Write a comment